This is a great post about this complex issue in US base Practice Management systems and EHRs …
Please ensure your adblock and popup block and other paranoia tools are in full effect before visiting the above site. It is chock-ablock full of malvertizing. I couldn’t read the article for all my analysis suite output telling me everything it was trying to do. For user agent Firefox, it will redirect you to vohchpg12.com where it plasters a big “critical firefox update” and tries to get you to download what is marked as a .js file. I just got out of there. I have well patrolled walls, but I would rather not come under siege.
I read that site every day without any issues like that.
Gave it another go. She says: Optimize your claim authorization process. Use claim scrubbing in your billing system. Preempt the claim scrubbing system by optimizing your workflow to produce clean results. Validate the scrubbing and workflow against value-based reimbursement.
Seems pretty basic, and obvious to some of us. Those of us who only bill medicaid in the southern US must have these items optimized to the Nth degree to be able to keep the doors open at all. Most standard medical practices fail at every level of the above, and whine about how hard it is to survive and how poor reimbursement is. Insurance companies do not generally have the holistic overview of their own processes at the organizational level. This is for three elegantly blended reasons: First, it takes brains to come up with such an optimization scheme and implement it. Second, brains like that cost money, as does changing anything. Third, they know that optimizing the system would only increase claim throughput. If a person is undergoing treatment, and some delay effectively reduces the number of visits from 3 to 2, that is a 50% savings that allows them to steal more money. This adds up, and the profits of this go straight to that top margin. This can be calculated to easily pay a semi-retired nurse 12 bucks and hour to sit on the HMO phone and inform the clinic staff “We appreciate your request to find out if John Doe has an insurance card that gives him 25% off of the 300% inflated bill. Please allow 4-6 weeks plus shipping and handling for your request to be processed. You may call after that to find your results. Please write down this ticket number…click.”
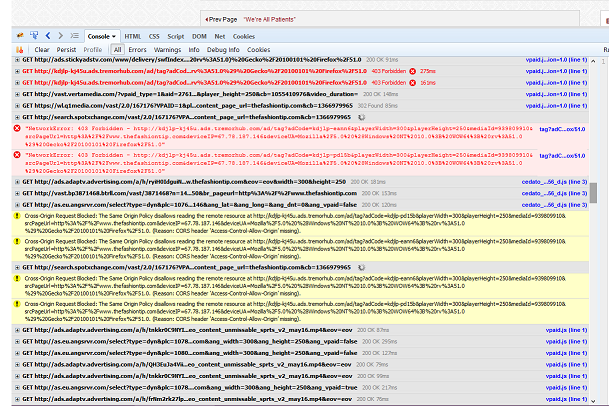
Huge scrollbar, and it wasn’t stopping. Massive lag too. -Just saying.
Also, why is this here and not public? We should default to public…
Couldn’t decide where it fit, so I defaulted to the lounge…
Development seems the best place IMHO.
To a developer, yes. Clinicians would see it as a “Practice Management” forum item.